Overcoming barriers to patient adherence: the case for developing innovative drug delivery systems
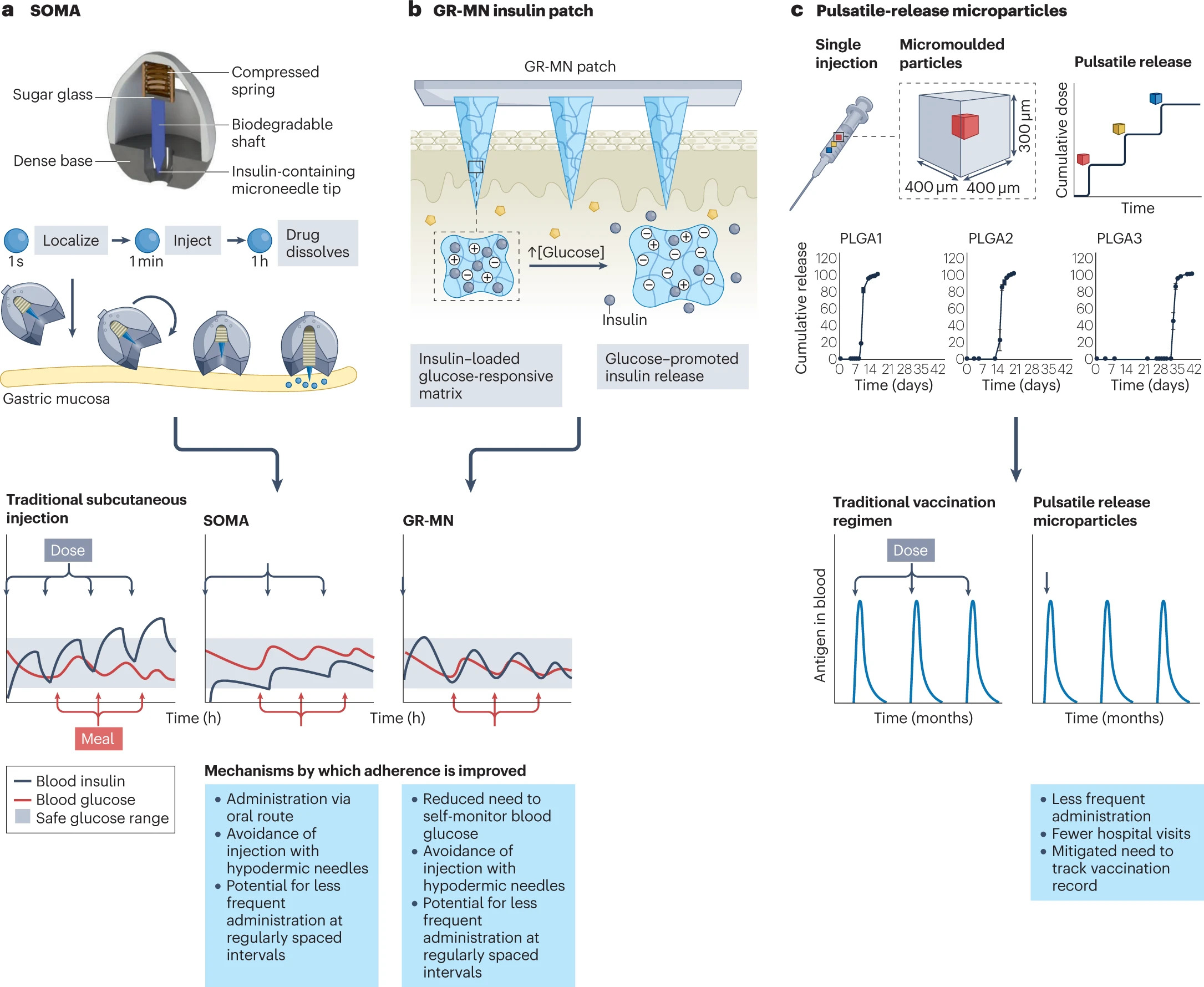
Poor medication adherence is a pervasive issue with considerable health and socioeconomic consequences. Although the underlying reasons are generally understood, traditional intervention strategies rooted in patient-centric education and empowerment have proved to be prohibitively complex and/or ineffective. Formulating a pharmaceutical in a drug delivery system (DDS) is a promising alternative that can directly mitigate many common impediments to adherence, including frequent dosing, adverse effects and a delayed onset of action. Existing DDSs have already positively influenced patient acceptability and improved rates of adherence across various disease and intervention types. The next generation of systems have the potential to instate an even more radical paradigm shift by, for example, permitting oral delivery of biomacromolecules, allowing for autonomous dose regulation and enabling several doses to be mimicked with a single administration. Their success, however, is contingent on their ability to address the problems that have made DDSs unsuccessful in the past.
Introduction
More than half of the world’s population takes at least one drug each day, and the demand for pharmaceuticals is only expected to increase as the global disease burden continues to grow1. The benefits that a drug seemingly affords in a highly controlled setting, however, will not translate to real-world use if patients do not take their medication as prescribed. Poor medication adherence is the most common reason for disparities observed between results obtained in randomized clinical trials (RCTs) and real-world outcomes2,3 and remains pervasive; estimates of non-adherence are around 50% for chronic illnesses4,5. In the United States alone, poor adherence is responsible for an estimated 125,000 deaths per year, a figure comparable with the number of deaths caused by colorectal cancer, breast cancer and prostate cancer combined6,7. Poor adherence is also estimated to cause 10% of all hospitalizations and underlie $100–300 billion of avoidable health-care costs annually owing to wasted medicine, unnecessary diagnostic procedures and excessive health-care provider utilization8,9,10. Rates of non-adherence are especially high among older people, who are more likely to require complicated treatment plans and suffer from cognitive and/or functional impairments (for example, dysphagia) that impede their ability to administer certain types of medication11. Owing to a globally ageing population and a worldwide shift in the general disease burden from acute to chronic conditions, the adverse effects of non-adherence are only expected to increase12.
The key reasons for poor adherence are patient forgetfulness, anxiety about treatment-associated adverse effects, low motivation due to a perceived lack of efficacy, poor health literacy and aversion to the health belief model, and stigmatization4,8. Other factors that may play a role include high prescription costs and insufficient patient–provider communication. Besides negatively impacting the health of an individual, pervasive non-adherence can have a pernicious effect on the health of a community, especially as it pertains to communicable diseases. For example, failing to complete a vaccination schedule or a course of antibiotics or antivirals as prescribed can lead to the emergence of a resistant strain of a contagious bacteria or virus. Vaccine refusal has been implicated in outbreaks of varicella, measles and pertussis, among others13.
Improving adherence is recognized as one of the most impactful and cost-effective strategies for improving the health of the general population, yet it has not garnered the same attention as other approaches for improving wellness4. A mere 1% increase in drug utilization among individuals enrolled in Medicare and Medicaid in the United States is estimated to result in a $3 billion reduction in national health-care spending (0.2% of the total Medicare and Medicaid budget in 2020 (ref. 14))15,16. Traditional health-care provider-mediated strategies for improving adherence by educating and empowering patients have produced inconsistent and often underwhelming results17 (Box 1). These interventions are often too complex, requiring health-care infrastructure and/or some extent of personalization, to be cost-effective at scale. Drug delivery systems (DDSs) are promising technological alternatives that can mitigate the logistical factors negatively impacting real-world adherence. DDSs are formulations, systems or technologies used to modulate the release of a drug in the body over time and/or target the drug to a particular tissue or cell type. The first DDS, a sustained-release system delivering dextroamphetamine, was approved in 1952 (Box 2). A timeline describing the development of several key DDSs — with an emphasis on those that did (or are expected to) improve medication adherence — is provided in Fig. 1.
In this Review, we first overview the fundamentals of DDSs and the mechanisms by which they can improve adherence. We then summarize the impact that DDSs have had on patient adherence across four disease and intervention types: chronic, relapsing–remitting, acute and prophylactic. Finally, we discuss the lessons that can be learned from several novel DDSs that failed to realize broad commercial success.
Download the full review as PDF here: Overcoming barriers to patient adherence: the case for developing innovative drug delivery systems
or read it here
Baryakova, T.H., Pogostin, B.H., Langer, R. et al. Overcoming barriers to patient adherence: the case for developing innovative drug delivery systems. Nat Rev Drug Discov 22, 387–409 (2023).
https://doi.org/10.1038/s41573-023-00670-0
Read more about Insulin
Read more about the World Asthma Day: