Colonic drug delivery: Formulating the next generation of colon-targeted therapeutics
Abstract
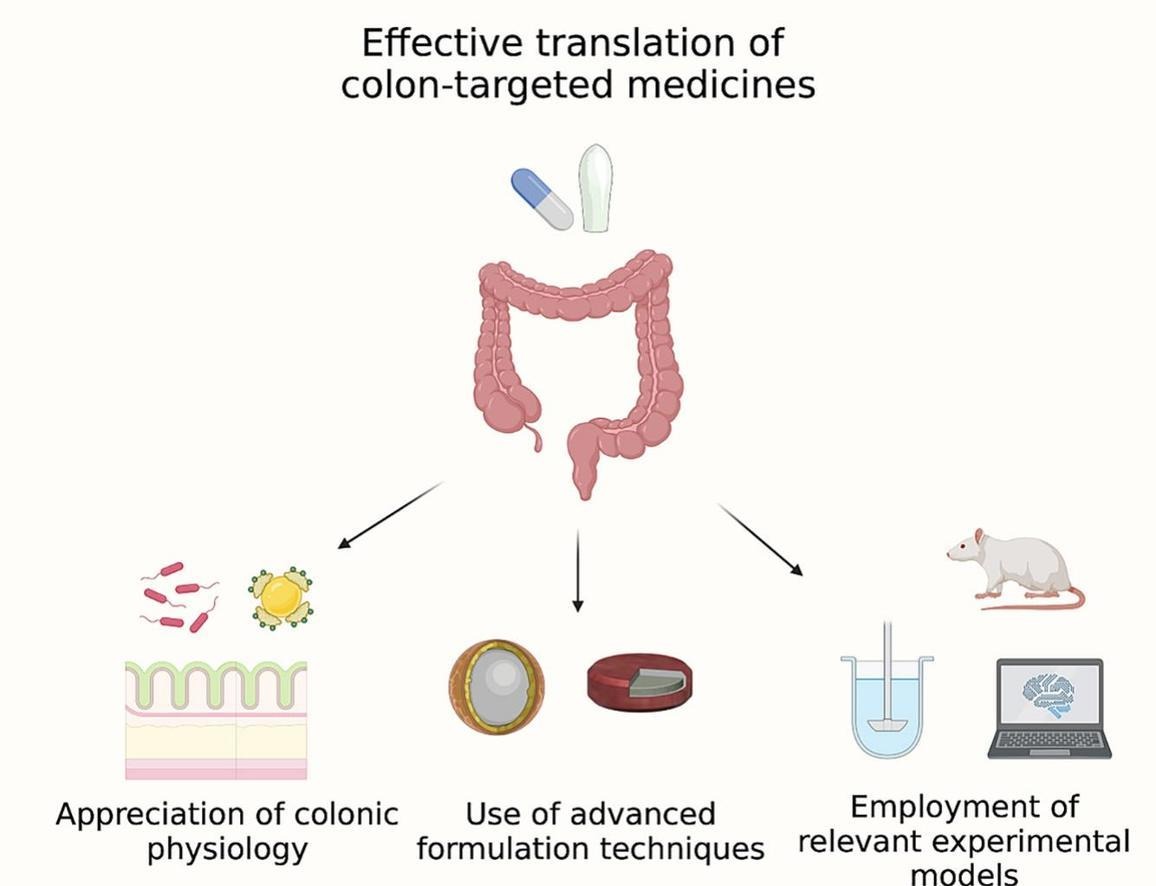
Colonic drug delivery can facilitate access to unique therapeutic targets and has the potential to enhance drug bioavailability whilst reducing off-target effects. Delivering drugs to the colon requires considered formulation development, as both oral and rectal dosage forms can encounter challenges if the colon’s distinct physiological environment is not appreciated. As the therapeutic opportunities surrounding colonic drug delivery multiply, the success of novel pharmaceuticals lies in their design. This review provides a modern insight into the key parameters determining the effective design and development of colon-targeted medicines. Influential physiological features governing the release, dissolution, stability, and absorption of drugs in the colon are first discussed, followed by an overview of the most reliable colon-targeted formulation strategies. Finally, the most appropriate in vitro, in vivo, and in silico preclinical investigations are presented, with the goal of inspiring strategic development of new colon-targeted therapeutics.
1. Introduction
Colonic drug delivery is experiencing a renaissance due to the multitude of associated pharmaceutical benefits and opportunities discovered in recent years [1]. Targeting drugs to the colon can enable superior treatment of local diseases, access to local therapeutic targets, reductions in systemic drug exposure and associated toxicity, and even improvements in drug bioavailability [[2], [3], [4]]. Traditionally, colonic drug delivery has focused primarily on local diseases, such as inflammatory bowel disease (IBD) and colorectal cancer [5,6]. Colonic drug delivery can improve the treatment of local diseases by optimising drug concentration at the target site whilst limiting systemic exposure [7,8]. Increasing characterisation of the colonic and rectal environments has led to the recognition of new local targets, such as the microbiome, enteric immune system, and lymphatic system [9,10]. These emerging targets not only allow treatment of colonic pathologies but may facilitate treatment of systemic conditions and those affecting distal organs [[11], [12], [13]]. For example, the intestinal microbiome has been discovered to modulate traumatic spinal cord injury, dyslipidaemia, urinary tract infections, and even neurological conditions, such as Alzheimer’s and Parkinson’s disease [[14], [15], [16], [17], [18]]. Moreover, the mesenteric lymphatic system could be targeted to treat insulin resistance and facilitate access to the brain [19,20]. This expansion in potential therapeutic targets, coupled with advancements in pharmaceutical sciences, has led to heightened interest in colonic delivery of new treatment modalities, including probiotics, postbiotics, vaccines, oligonucleotides, and biologics [[21], [22], [23], [24], [25]].
The first case of colonic drug delivery was sulfasalazine, a prodrug that was introduced for the treatment of IBD in 1941 [26]. Sulfasalazine is composed of the active 5-aminosalicylic acid (5-ASA, mesalamine, mesalazine) linked to the carrier molecule sulfapyridine through an azo bond [27]. Sulfasalazine is activated in the colon by bacteria that cleave its azo bond, releasing 5-ASA for local treatment of inflammation. Whilst sulfasalazine has remained an effective IBD treatment for almost a century, around half of patients report allergic reactions or other adverse events following its use [28]. These observations have been associated with the sulfapyridine component of the prodrug [29], sparking subsequent development of other 5-ASA prodrugs, including olsalazine and balsalazide [30,31]. The prodrug strategy is still utilised for colonic delivery, for example an azo prodrug of tofacitinib was recently shown to effectively treat a mouse model of IBD [32]. Similarly, gut restriction of molecules (particularly peptides) could enable local colonic action by preventing systemic absorption [33]. However, design of prodrugs/gut-restricted therapeutics is drug-specific and can require lengthy regulatory approval [34]. This review will instead focus on formulation-based colonic drug delivery, as a single formulation can enable the colonic release of many diverse types of drugs. Further, modified-release formulations of approved drugs can achieve faster market authorisation as they do not need to repeat studies proving the intrinsic drug properties, such as toxicity or pharmacology [35].
Formulations that enable colonic drug delivery include orally administered dosage forms with colon-specific release and those that are administered via the rectum. The first formulation enabling targeted drug delivery to the terminal ileum/proximal colon (also known as ileocolonic delivery) via the oral route was published in 1982, constituting a pH-sensitive methacrylate polymer marketed as Eudragit® S (Evonik) [36]. Eudragit® S is a synthetic copolymer composed of poly(methacrylic acid, methyl methacrylate) at a ratio of 1:2 that dissolves when intestinal pH exceeds 7.0 [37]. As such, Eudragit® S is used as an enteric coating for oral dosage forms designed to release drugs in the terminal ileum. To date it is a prevalent technology that has been incorporated in several marketed formulations, notably those intended to deliver mesalazine to the colon for the treatment of IBD, such as Asacol® (Tillotts Pharma) and Lialda®/Mezavant® (Cosmo Pharmaceuticals). However, the reliability of pH-sensitive polymers for colonic drug delivery has been called into question for some time [1,37,38]. Human studies have found enteric coatings to show inconsistent release patterns, with coatings dissolving prematurely or remaining intact in some individuals [39,40]. This inconsistency arises from variability in intestinal pH and leads to a proportion of patients not receiving the intended dose of their prescribed drug. Further, the disease pathophysiology can increase the risk of enteric coating failure; for example, in IBD intestinal pH is often markedly lower than in healthy individuals [41].
Other mechanisms for achieving colonic drug delivery can similarly present variable release profiles in patients. For example, the time-based approach to accessing the colon via the oral route can be highly affected by variability in gastrointestinal (GI) transit time. Time-based formulation approaches utilise systems that are triggered upon ingestion (e.g., by exposure to GI fluids or low gastric pH) to begin a lag phase that should last until the dosage form enters the colon where site-specific drug release occurs [1,6,42]. However, many factors, including presence of disease, surgery, concurrent medications, or a change in diet, can alter patients’ GI transit times and lead to time-based approaches failing to predictably deliver drugs to the colon [43]. Related challenges may be observed with microbiota-dependent systems, which utilise coatings that remain intact in the proximal GI tract and are digested by colonic bacterial enzymes. Upon coating digestion, site-specific drug release should occur, forming the basis for this colon-targeting strategy [[44], [45], [46]]. Polysaccharides are common materials used for microbiota-triggered colonic drug delivery as they are indigestible by human enzymes and degraded by the majority of the population’s microbiota due to broad expression of bacterial polysaccharidases [47,48]. That said, if the colonic microbiome becomes significantly perturbed (e.g., following antibiotic administration or due to severe disease), then there is a risk that polysaccharidases will not be produced in sufficient concentrations for coating digestion [49]. Ultimately, this would lead to dosage forms being excreted intact within stool without releasing their drug cargo. In recognition of the unpredictability of relying on one physiological stimulus for colonic drug release, several advanced multi-faceted technologies have been developed in recent years [1]. Newly licensed technologies have provided dependable colonic drug delivery in clinical studies [50,51]; these advances are now revolutionising how orally administered, colon-targeted systems are developed and have opened numerous therapeutic opportunities for the field.
Rectal drug delivery encompasses different advantages and disadvantages compared to colonic delivery via the oral route. For one, rectal formulations are less affected by inter- and intra-patient physiological variability as they do not need to transit the upper GI tract before reaching the colon. In an empty state, the rectal environment is relatively stable, thus facilitating predictable drug release and absorption [52]. Further, the rectal route can be advantageous for the delivery of drugs that have unpleasant taste profiles, cause GI irritation, are unstable in the upper GI tract or undergo significant hepatic first pass metabolism [53]. The rectal route may also be beneficial in situations when safe swallowing is impaired, for instance due to dysphagia, unconsciousness, or in patients at extremes of age [54]. Despite these advantages, rectal formulations are generally less accepted than oral formulations for reasons including cultural preconceptions, invasiveness, and ease of administration. Mechanistically, rectal formulations can also face retention challenges and generally cannot deliver drugs beyond the colon’s splenic flexure [52]. For this reason, they are typically best suited for treating pathologies local to the distal colon and rectum, though systemic products such as vaccines have begun to be explored [55,56]. Rectal formulations can take several identities, most commonly suppositories, enemas, foams, and gels. Traditionally, rectal administration has focused on the delivery of small molecule drugs in simple solutions, emulsions, or suspensions for treatment of constipation, IBD, haemorrhoids, pain, or nausea and vomiting [52]. However, in recent years more varied and advanced formulations have been investigated both preclinically and in trials, which can serve as inspiration for how the potential of the delivery route may be maximised [[57], [58], [59], [60]].
This review provides a timely update on the most effective strategies for developing new colon-targeted treatments. A detailed evaluation of the colonic environment will first be presented to facilitate strategic formulation design. Next, techniques underpinning multi-stimuli targeting technologies will be discussed, with specific attention cast on mechanisms with reliable in vivo performances. The review will conclude with an overview of the pertinent preclinical investigations for novel colon-targeted medicines, highlighting the most appropriate in vitro, in silico, and in vivo models to select when translating new treatments.
Download the full review as PDF here: Colonic drug delivery: Formulating the next generation of colon-targeted therapeutics
or read it here
Excipients mentioned in the study besides other: Eudragit S 100, Eudragit RS, HPMC, Starch, PEG
Laura E. McCoubrey, Alessia Favaron, Atheer Awad, Mine Orlu, Simon Gaisford, Abdul W. Basit, Colonic drug delivery: Formulating the next generation of colon-targeted therapeutics, Journal of Controlled Release, Volume 353, 2023, Pages 1107-1126, ISSN 0168-3659, https://doi.org/10.1016/j.jconrel.2022.12.029.

