Formation of N-Nitrosamine Drug Substance Related Impurities in Medicines: A Regulatory Perspective on Risk Factors and Mitigation Strategies
Abstract
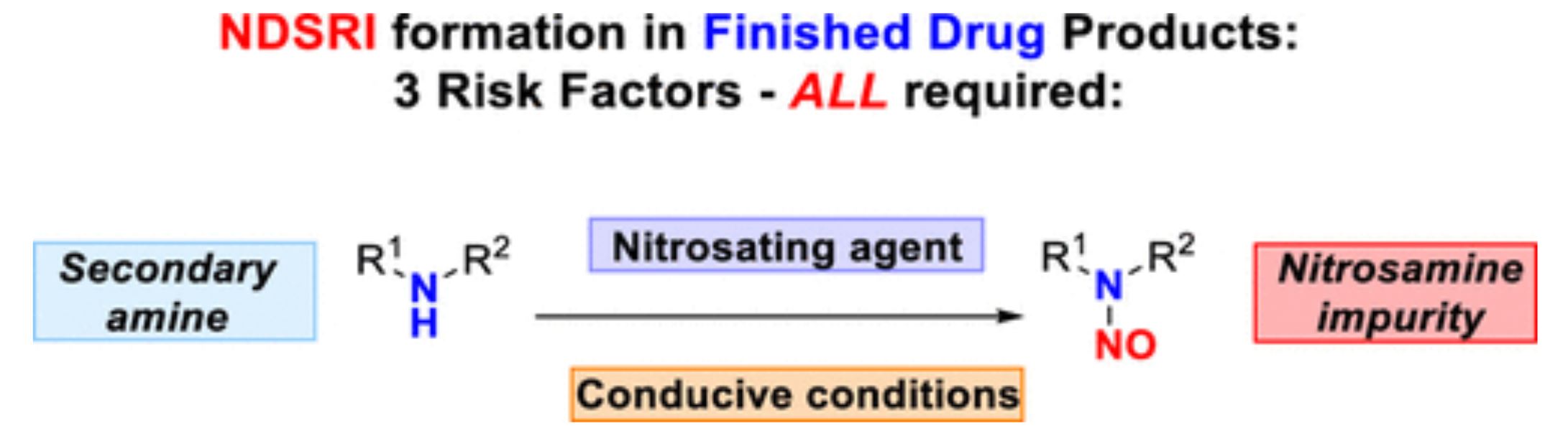
The detection of N-nitrosamine impurities in medicines and the recent emergence of nitrosamine drug substance related impurities (NDSRIs) has posed a great challenge to manufacturers of drug products and regulators alike. NDSRIs are primarily associated with reactions occurring in the drug product which brings particular complexity. This paper will explore the current technical knowledge surrounding the formation of these impurities, including the risk factors, reaction conditions, and potential mitigation strategies. Scientific understanding of these areas is still evolving, and we will highlight both the scientific progress made and discuss the significant gaps in mechanistic knowledge still remaining. These gaps render accurate predictions of NDSRI formation extremely challenging. The pharmaceutical industry should continue to work on potential mitigation strategies and generation of additional scientific data to address the mechanistic gaps. Regulatory guidance and policy will continue to advance and adapt in response to further changes in scientific understanding.
Introduction
N-Nitrosamines are a class of organic impurities that includes highly potent mutagenic substances which are classified as probable human carcinogens. (1) Isolated reports of N-nitrosamine impurities in medicines were documented in the past, (2) however reports on the detection of N-nitrosodimethylamine (NDMA) in valsartan drug substance from one manufacturer in June 2018 led to a series of regulatory actions including market recalls and an Article 31 of Directive 2001/83/EC referral procedure in the EU. (3) That scientific review was subsequently extended to other drug substances in the “sartan” class on the basis of similar structural features and synthetic processes which implied a similar risk of generating N-nitrosamine impurities. In addition to NDMA, N-nitrosodiethylamine (NDEA) was subsequently discovered in some sartan medicines. The outcome of that scientific review was the requirement for marketing authorization holders (MAHs) of sartan medicines to apply strict limits for NDMA and NDEA in their release specifications.
In September 2019, a second Article 31 referral into the safety of medicines containing ranitidine began in the EU, following reports of the presence of NDMA above acceptable levels in ranitidine tablets. (4) The referral concluded that ranitidine medicines, used to treat heartburn and stomach ulcers, should be suspended until MAHs are able to demonstrate that the levels of NDMA can be controlled to acceptable levels throughout the assigned shelf life and that no further NDMA formation occurs in the body following ingestion. (5) The root cause of NDMA formation in ranitidine was subsequently reported to be the result of an intermolecular degradation of ranitidine without the requirement for any exogenous nitrite. (6)
In light of these reports and given the potential applicability of the identified root causes to other medicines, it was decided to conduct a more holistic review of N-nitrosamine impurities in medicines. The EU medicines regulatory authorities therefore conducted a scientific assessment (Article 5(3) opinion (7)) of N-nitrosamine impurities and considered the following aspects:
- Root causes for the formation of N-nitrosamines and measures to mitigate them.
- Methodology for defining acceptable limits for daily intake (AIs).
- Requirements for analytical methods to detect and quantify N-nitrosamine impurities.
- Risk for patients exposed to medicines containing N-nitrosamine impurities.
- The need for MAHs to evaluate the risk of presence of N-nitrosamines in the medicines and the extent of products in scope.
- The need for further nonclinical and clinical studies.
The assessment arrived at a range of conclusions in terms of known and suspected root causes, analytical method requirements, methodology for setting limits, and the need for further epidemiological studies. Up until that time, the majority of N-nitrosamine impurities in medicines had originated in the active substance manufacturing process. (8) As a result, the conclusions focused on how to manage highly potent small molecule N-nitrosamine impurities with published limits based on well-established toxicity data such as NDMA and NDEA. Nonetheless, the possibility of N-nitrosamine formation in drug products was highlighted based on the potential presence of nitrosating agents in excipients, water, and packaging components.
This led to a series of recommendations for dealing with N-nitrosamine impurities in medicines including:
- The need to mitigate the presence of N-nitrosamine impurities as much as possible.
- The need to establish appropriate control strategies for both active substances and drug products.
- The need for MAHs to conduct risk evaluations for the presence of N-nitrosamines in their products and to perform confirmatory testing if a risk is identified.
- The need to set specification limits for detected N-nitrosamines in the drug product by default, in line with published limits.
- Considerations for analytical method development and sensitivity requirements.
- Control options when more than one N-nitrosamine is present in the same product.
- Methodology for setting limits for new N-nitrosamines with insufficient toxicity data including the establishment of a class-specific limit of 18 ng/day.
- Exceptions for medicines indicated for treatment of advanced cancer or where the active substance itself is genotoxic at therapeutic concentrations.
- Exceptional and temporary use of higher limits for products containing N-nitrosamine impurities above the acceptable intake but which still have a positive benefit/risk ratio.
- The need for further epidemiological studies.
This paper focuses on the scientific understanding related to risk factors for N-nitrosamine formation in medicines, including developments since the conclusion of the Article 5(3) opinion, (7) and highlights areas where further scientific investigations are required.
Download the full article as PDF here: Formation of N-Nitrosamine Drug Substance Related Impurities in Medicines_A Regulatory Perspective on Risk Factors and Mitigation Strategies
or read it here
Formation of N-Nitrosamine Drug Substance Related Impurities in Medicines: A Regulatory Perspective on Risk Factors and Mitigation Strategies, Răzvan C. Cioc, Ciarán Joyce, Monika Mayr and Robert N. Bream, Cite this: Org. Process Res. Dev. 2023, Publication Date:July 21, 2023, https://doi.org/10.1021/acs.oprd.3c00153, © 2023 The Authors. Published by American Chemical Society
Watch for free our webinar “Antioxidants, a safe and viable Inhibition Strategy for Nitrosamine Formation In Drug Products” here:


