Substrate-free dissolving microneedles with barbed shape to increase adhesion and drug-delivery efficiency to skin
Abstract
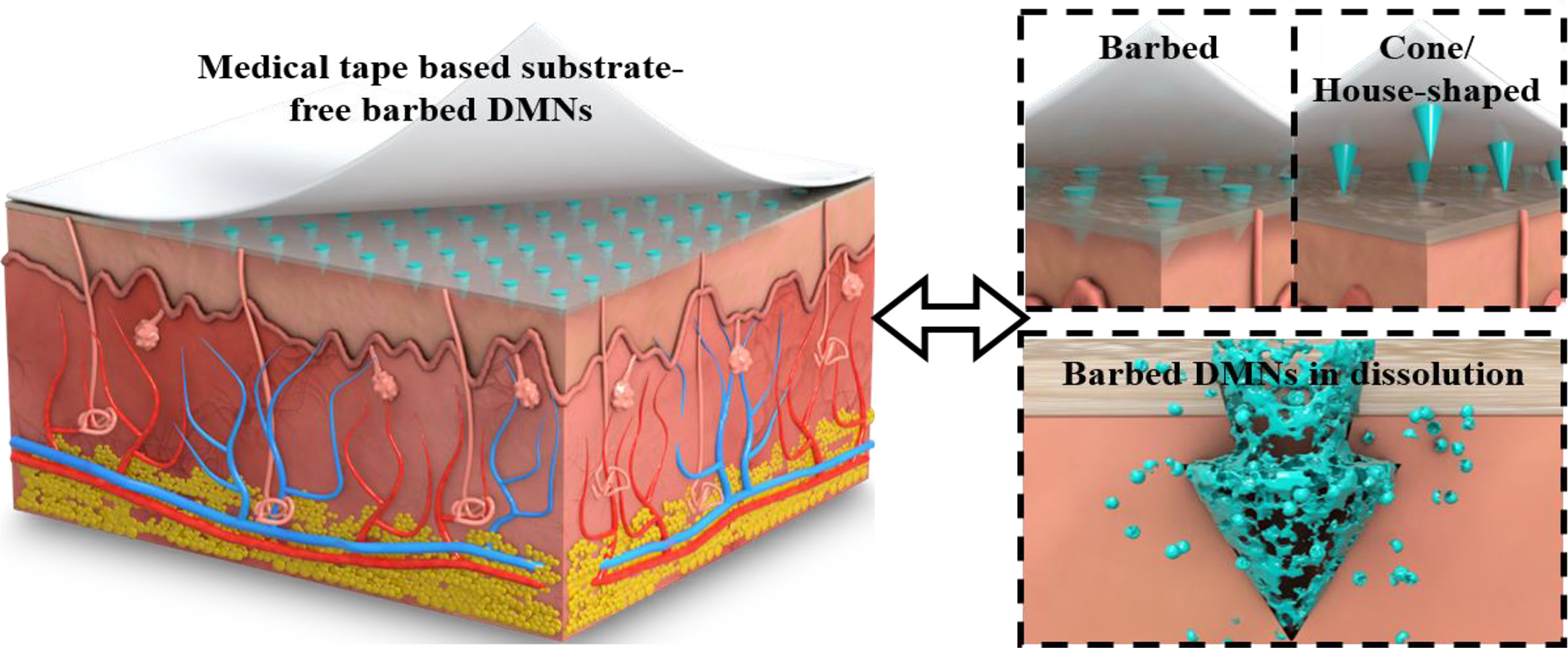
Microneedle drug delivery has recently emerged as a clinical method, and dissolving microneedles (DMNs) offer exclusive simplicity and efficiency, compared to the other kinds of microneedles. The tips of most currently available DMNs are cone/house-shaped to result in a lower penetration force. Penetration of the needle tips into the skin relies mainly on the back tape or external pressure, and their adhesion to the skin is relatively low. In addition, only the drug in the part of tips that are pierced into the dermis can be dissolved, resulting in drug waste. Inspired from the barbed structure of the honeybee stinger, we reported substrate-free DMNs with a barbed structure by a dual-molding process, which is suitable for mass production. Those DMNs showed 3-fold greater adhesion force between the needle tips and the skin, better dissolution and deeper penetration than house-shaped DMNs in vivo under the same conditions. For the in situ treatment of psoriasis in mice, the barbed DMNs required only the half dose of house-shaped DMNs to achieve similar efficacy.
Introduction
Psoriasis is a chronic, multi-system inflammatory skin disease with a long disease cycle, risking recurrence or almost lifelong, which has a great impact on the patient’s physical health and mental condition1–2. Clinical manifestations are dominated by erythema and fresh flakes, and all parts of the body may become the onset site3. Most of the patients are young adults, and the probability of the disease is similar between men and women4. Depending on the severity of the disease, appropriate measures are taken. The first consideration is topical therapies, including retinoids and vitamin D3. These topical medications are effective and can be administered in compliance with a doctor’s prescription5. Due to the molecular properties of some medications, direct topical application may make it difficult for the medication to enter the subcutaneous tissues to work, resulting in poor utilization of the medication. In more severe cases, a combination of oral therapy with methotrexate and cyclosporine may be considered6–7. Drug utilization is also poor with oral administration given the risk of hepatic and renal degradation8–10. Therefore, owing to the drawbacks and problems of the above routes of administration, a new route of administration, topical administration through microneedles, has been proposed to improve drug utilization and efficiency based on topical administration, such as 11–15.
Microneedles have been widely reported for drug delivery20–22 to replace topical, oral, intramuscular and intravenous delivery, each of which has its own advantages and disadvantages16–19. The principle of microneedle drug delivery is to use microneedle array to puncture the skin and then directly release the drug into the subcutaneous tissue to exert the drug effect, which has been popularized because of its simple operation, rapidity and efficiency. In addition, subcutaneous tissue has a strong immune cell population and unique pharmacokinetics23, which can achieve the full utilization of the drug and largely enhance the drug utilization. In addition, due to the role of subcutaneous tissue immune cell population, microneedle drug delivery shows similar efficacy to intramuscular injection, reducing the use of sharp needles, largely avoiding the spread of disease through syringe needles, and having better generalizability. In addition, the production process of microneedles is relatively simple and has the potential to satisfy batch production. Microneedle drug delivery is characterized by minimal pain, no bleeding, and self-operation without involvement of professional sites and professionals, thus it has a wide range of application scenarios and is expected to become a mainstream method.
There are four main types of microneedles used for drug delivery: solid microneedles, coated microneedles, hollow microneedles, and dissolving microneedles (DMNs). Here is their brief introduction: solid microneedles are only used to puncture the skin, after which the microneedles are removed. Subsequently, some tiny holes are created in the skin, and then the drug will be applied to the skin surface, penetrate through the holes into the subcutaneous tissues to play a role. Due to the intrinsic function of the skin, the tiny holes will close within a certain period of time, when the diffusion of the drug will be hindered. Therefore, the drug delivery efficiency of solid microneedles is relatively low. Coated microneedles is encapsulated with a layer of drug on the surface and deliver the drug directly to the subcutaneous tissue through external force.
The drug delivery efficiency of the coated microneedle is slightly improved compared to the solid microneedle, but the volume of the delivered drug is still low. Hollow microneedles24–30, which are the miniaturized and arrayed traditional syringes, deliver relatively substantial amounts of drug solutions into subcutaneous tissues by external pushing force after piercing the skin,. Most of the existing preparation parties are relatively complex processes such as photolithography and laser etching, which limits the development of hollow microneedles. DMNs are composed of a mixture of a drug and a biodegradable polymer that is cured31–35. After pierced the skin, the DMNs dissolve under the action of subcutaneous tissue fluid, and then release the drug. DMNs are simple to prepare with mass production, and can reduce sharp waste emissions. In addition, DMNs are easy to administer, for they can be pressed for a few minutes after puncture to realize dissolution and drug delivery. The amount of drug can meet most of the needs, such as delivery of vaccines36–40, treatment of diseases, and so on41–45. Therefore, DMNs are most widely used and researched.
DMNs are mainly cone/house shaped in order to have a small piercing force to pierce the skin. The preparation method is mainly a dual-molding process. The master mold is prepared by 3D printing or silicon processing, after which PDMS is poured as the negative mold. Then, the mixed solution of the drug and dissolvable polymer carrier is added onto the PDMS mold, and the DMNs will be formed after curing. The above conventional preparation methods have the following obvious drawbacks: (1) Only a part of microneedles pierced the skin are able to be dissolved of the drug in the substrate is wasted, because it remains out of the skin. (2) The adhesion between the DMNs and the skin is weak, and any movement of the skin may cause the needles to partially slip out, leading to incomplete dissolution (Fig. 1A).
Therefore, based on the consideration of the above problems and inspired by the bee stinger structure, we envisioned a substrate-free barbed DMNs based on medical tape, which can avoid the waste of drugs in the substrate and enhance the adhesion between the needle tips and the skin. Although some barbed structures are reported, their complicated fabrication process or high cost is not suitable for practical application of DMNs. Current methodologies primarily center on 3D printing and supplementary procedures in the context of microneedle fabrication. Precision in structuring and orienting the barbs is achieved through the application of a magnetic field during the 3D printing process for microneedles46–47. Additionally, meticulous control of the exposure time during 3D printing provides a means to modulate the morphology of the barbs48. Alternatively, sequential steps, such as thermal expansion, are employed for precise control over the barbs’ morphology49. Although Li et al.’s team prepared barbed DMNs by the dual-molding process, it seems that the situation of drug loading on the substrate has not been solved, i.e., the drug utilization has not been well improved50.
To the aforementioned disadvantages, we prepared for the first time a substrate-free barbed DMNs based on the dual-molding process (Fig. 1B). We chose the in situ treatment of psoriasis on the back of mice as an experimental model, and the substrate-free barbed DMNs required only half of the amount of house-shaped DMNs to achieve similar efficacy with fewer associated side effects. The result verified the practical usefulness of the substrate-free barbed DMNs, and is expected to play a important role in the field of drug delivery.
Read more here
Yingjie Ren, Kaiming Yang, Zhongyan Wang, Zhitong Zhang, Yufeng Chen, Xiaoyi Shi, Jiayan Zhang, Yuxuan Chen, Dong Huang, Junshi Li, Zhihong Li, Substrate-free dissolving microneedles with barbed shape to increase adhesion and drug-delivery efficiency to skin, Journal of Controlled Release, Volume 368, 2024, Pages 199-207, ISSN 0168-3659, https://doi.org/10.1016/j.jconrel.2024.02.009.
Read also the current articles on Microneedles here:
- Polymeric microneedles for the eye
- Hypericin emulsomes combined with hollow microneedles as a non-invasive photodynamic platform for rheumatoid arthritis treatment
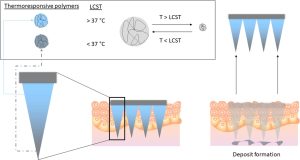
- Leveraging novel innovative thermoresponsive polymers in microneedles for targeted intradermal deposition