Cancer nanomedicine: emergence, expansion, and expectations
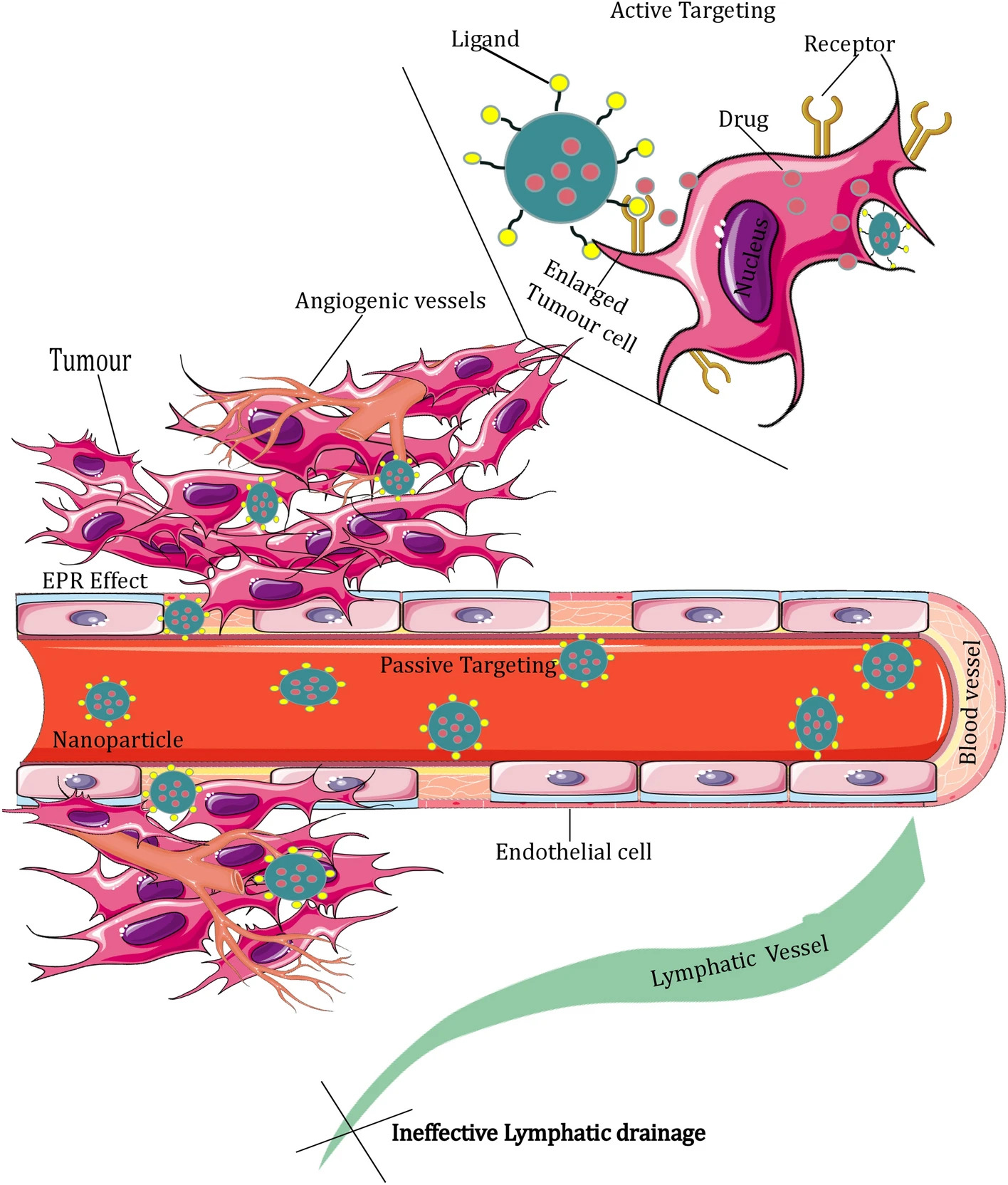
The introduction of cancer nanomedicine has substantially enhanced the effectiveness of cancer treatments. Nano-formulations are becoming more prevalent among other treatment methods due to their improved therapeutic efficacy and low systemic toxicity. The discovery of the enhanced permeability and retention (EPR) effect has led to the development of numerous nanodrugs that passively target tumours. Then researchers identified certain cancer cells overexpress certain receptors, targeting these over-expressing receptors using targeting moiety on the surface of the nanoparticles becomes promising and surface functionalization of nanoparticles has become an important area of cancer nanomedicine. This leads to the physiochemical modification of nanoparticles for strengthening the EPR effect and active targeting. This review comprehensively outlines the origins of cancer nanomedicine, the role of the EPR effect, the tools of nanotechnology and their specifications, and the nature of passive and active targeting, which gives important direction for the progress of cancer therapy using nanomedicine. The review briefly enlists the available nano formulations for different cancers and attempts were made to account for the barriers to clinical translation. The review also briefly describes the transition of research from nanomedicine to nano-immunotherapy.
1 Introduction
Cancer nanomedicine is at a point of debate when we collectively analyze the past 15 years of its growth and contribution to medicine. Recent discussions have conveyed that the influence of nanotechnology is supreme in the research world, but its societal impact on health and translation from research to product is very minimal. Dr Kinam Park remarked in the cover story of the Journal of control release that the nanomedicine hype is close to an unfortunate end by quoting the announcement of the US National Cancer Institute (NCI) about the stoppage of funding for its Centres of Cancer Nanotechnology Excellence (CCNEs) [1]. However, the revolutionary 60-year journey and the shift from Feynman’s nanotechnology [2] to Metchnikov and Ehrlich’s nanomedicine should not go unnoticed. The shift in using nanomedicine for cancer therapy is promoted by the introduction of Professor Maeda’s enhanced permeability and retention (EPR) effect. It was a pioneering concept in the 1980s [3] and found its way to clinical use over the last three decades. Most of the commercialized nanodrugs for cancer treatment entirely use the special transport capabilities made possible by the EPR effect to enter the tumour and exert an anticancer impact. From the very primitive Doxil (1995) to the modified multi-drug Vyxeos (2017) and Hensify (2019), nanomedicine substantiates its significance over conventional therapies for cancer.
The meritorious benefits of nanodrugs can only be revealed when compared to traditional tumour treatment methods. Since the most widely used chemotherapy agents fail to differentiate between normal and cancerous cells [4], patients are more likely to experience treatment failures as well as undesirable side effects. Initially, the nanomedicine used for cancer treatment was based on its enhanced accumulation in the tumour site because of the leaky vasculature, poor lymphatic drainage, and tumour microenvironment factors that promote cellular permeability. Apart from passive choosing, the exclusive and active targeting of tumour cells by nanodrugs [5] was initiated in the noughties with the utilization of targeting moieties like antibodies, aptamers, ligands, peptides, etc. Modern antibody technology joined hands with nanomedicine to use monoclonal antibodies [6] and small antibody constructs for targeting specific cell surface markers in tumour cells. Concurrently, ligand-based targeting has also progressed well. The overexpression of transferrin [7, 8], folate [7, 9], and integrin [10, 11] receptors served as tumour cell surface markers, and ligands for the same were employed to synthesize surface-functionalized nanoformulations [7,8,9,10, 12,13,14]. All these biggest expansions in nano-based cancer therapies for the past 20 years are remarkable and designated as the “golden era” of cancer clinical trials.
The evolution of cancer nanomedicine is like an ocean being filled drop-by-drop. Its genesis is grateful to the contributions of chemistry, polymer science, biophysics, and molecular biology. The power and popularity of nanodrugs in cancer treatments have been revealed by the 20,300 publications in the last year and the 192 active clinical trials around the world. The sixth-most significant growth technology to monitor over the next 10 years, according to Forbes in 2021, is nanotechnology. In this review, we will showcase the entry of nanodrugs in cancer treatment, their superiority over conventional therapies, available nano-formulations, ongoing developments, and the drawbacks of existing systems while exploring different types of nanoparticles and their features.
Download the full study as PDF here: Cancer nanomedicine: emergence, expansion, and expectations
or read it here
Kizhakkanoodan, K.S., Rallapalli, Y., Praveena, J. et al. Cancer nanomedicine: emergence, expansion, and expectations. SN Appl. Sci. 5, 385 (2023).
https://doi.org/10.1007/s42452-023-05593-4

