Nanocarriers in Tuberculosis Treatment: Challenges and Delivery Strategies
Abstract
The World Health Organization identifies tuberculosis (TB), caused by Mycobacterium tuberculosis, as a leading infectious killer. Although conventional treatments for TB exist, they come with challenges such as a heavy pill regimen, prolonged treatment duration, and a strict schedule, leading to multidrug-resistant (MDR) and extensively drug-resistant (XDR) strains. The rise of MDR strains endangers future TB control. Despite these concerns, the hunt for an efficient treatment continues. One breakthrough has been the use of nanotechnology in medicines, presenting a novel approach for TB treatment. Nanocarriers, such as lipid nanoparticles, nanosuspensions, liposomes, and polymeric micelles, facilitate targeted delivery of anti-TB drugs. The benefits of nanocarriers include reduced drug doses, fewer side effects, improved drug solubility, better bioavailability, and improved patient compliance, speeding up recovery. Additionally, nanocarriers can be made even more targeted by linking them with ligands such as mannose or hyaluronic acid. This review explores these innovative TB treatments, including studies on nanocarriers containing anti-TB drugs and related patents.
Introduction
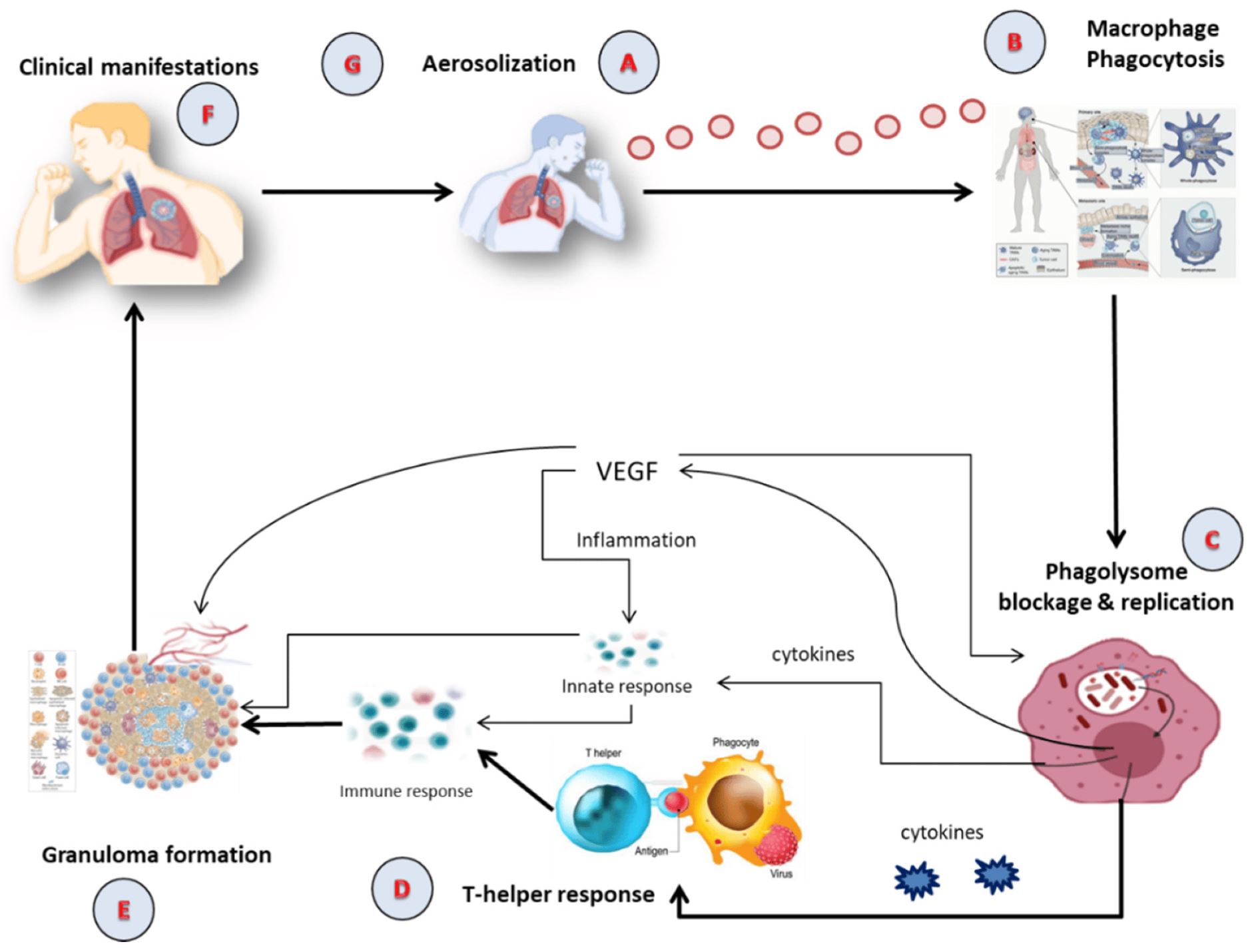
Among the most important global health challenges are infectious diseases such as tuberculosis (TB), acquired immunodeficiency syndrome, and human immunodeficiency virus infection [1,2]. Mycobacterium tuberculosis, an aerobic, Gram-positive, non-motile, acid-fast tubercular, rod-shaped bacillus, causes airborne TB, which mostly affects the lungs but may also impact extra-pulmonary regions [3]. Due to their lipid-rich cell walls, mycobacteria may live within alveolar macrophages [4]. The tubercle bacillus, M. tuberculosis, which is spread via airborne droplets and can remain, live, and divide every 16–20 h inside alveolar macrophages, is the principal method of transmission for this dangerous illness [5]. Per the latest report by World Health Organization (WHO), about 10.6 million cases of TB were reported in 2021, comprising 6 million men, 1.2 million children, and 3.4 million women [6]. It was estimated that about 1.6 million people died from TB in 2021 throughout the world. About 80% people infected by TB reside in low- and middle-income countries. The main causes for TB include weakened immune system, chewing of tobacco, undernourishment, and other complications such as diabetes and HIV infection [6]. In 2021, 2.2 million new TB cases were attributed to undernourishment, 740,000 to alcohol use disorders, and 690,000 to smoking throughout the globe. To reach the global goal set at a high-level UN meeting on TB in 2018, USD 13 billion is required annually for TB prevention, diagnosis, treatment, and care. It is expected that TB detection and treatment saved 74 million lives between 2020 and 2021 [7]. TB is the second highest infectious cause of death after COVID-19 and the thirteenth major cause of mortality across the world [8]. TB exists in all nations and among all age groups, but it can be treated and avoided. One of the Sustainable Development Goals (SDGs) of the United Nations is to end the TB epidemic by 2030 [9].
Chemotherapy is currently the only option for the clinical management of TB patients, with cure rates of up to 95% when given correctly to those with drug-susceptible TB. However, the majority of anti-TB medicines have subpar pharmacokinetic characteristics, which frequently prevent them from performing to their full potential in clinical situations [10]. Poor bioavailability due to variable drug absorption and unwanted first-pass metabolism, lengthy regimens with high dosing frequencies, and individual and combined drug toxicity as well as severe adverse effects are some of the issues related to the therapeutic limitations of the current anti-TB regimens. These challenges contribute to low patient adherence, therapeutic failure, and the alarming emergence of multidrug-resistant (MDR) strains, all of which explain TB’s current lethal state and the pressing need to advance anti-TB treatment [11,12].
Advanced drug delivery systems require the development of a nanotechnological technique, which is a rapidly evolving cutting-edge scientific field that includes a wide range of disciplines such as chemistry, physics, and biology as well as special nanodimension structures with therapeutic applications in pharmacology and the biomedical field [13]. Many researchers are interested in the development and standardization of nanocarriers for various reasons, such as reduction in drug doses, minimal adverse effects, solubility and bioavailability improvement of drugs, targeted drug delivery resulting in improved patient compliance, and acceleration in recovery of patients [14,15]. These nanocarriers include solid lipid nanoparticles, nanostructured lipid carriers, liposomes, nano-emulsion, nanosuspension, nanoparticles, polymeric micelles, and dendrimers [16]. The nanocarriers appear to be a viable and intriguing approach to solve the limitations associated with conventional treatment associated with TB [17].
Besides the above mentioned treatment, vaccination is also another option for prevention of TB [18]. The WHO advises that, despite the Bacille Calmette–Guerin (BCG) vaccine’s success in preventing TB and reducing mortality among infants and young children who have received vaccinations since birth, it is important to take into account the vaccine’s capacity to produce “trained immunity” by causing non-specific immune sensitization to other pathogens [19]. Additionally, it might aid in lowering the prevalence of infectious diseases, such as malaria, that are resistant to antimicrobials. Several benefits, including the large surface area of the sub-micron-sized particles, increased interaction of the vaccine with the large surface area of the respiratory mucosa and enhanced penetration into bacilli-loaded granulomas attributed to nanotechnology-based approaches, may particularly benefit in targeting the most common respiratory forms of TB against which BCG appears to be ineffective [20]. Previous research has shown the ability of the antigens implanted on nano-particulate platforms to improve immune response to other pathogens causing other infectious diseases, indicating the possibility of TB vaccines having the same capability once created [21].
Download the full article as PDF here Nanocarriers in Tuberculosis Treatment Challenges and Delivery Strategies
or read it here
Excipients mentioned in the study: Compritol 888, Witepsol, Gelucire
Kumar, M.; Virmani, T.; Kumar, G.; Deshmukh, R.; Sharma, A.; Duarte, S.; Brandão, P.; Fonte, P. Nanocarriers in Tuberculosis Treatment: Challenges and Delivery Strategies. Pharmaceuticals 2023, 16, 1360. https://doi.org/10.3390/ph16101360
See the webinar:
“Enhanced Stability and Bioavailability of Poorly Soluble APIs“,
18 October 2023:
Get more information & register here for free:


