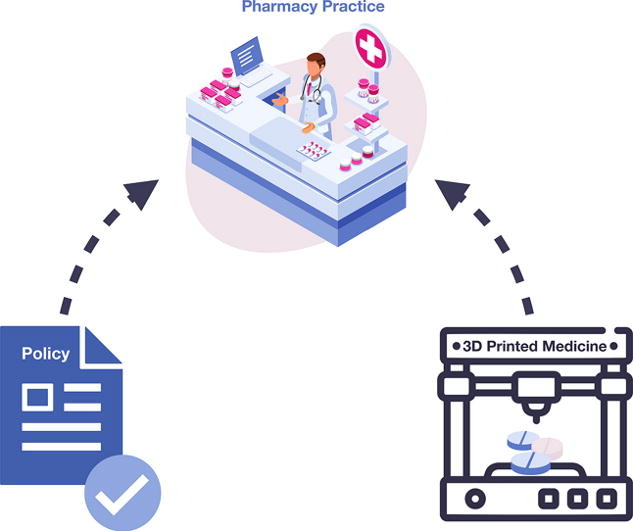
3D Printing for Personalised Medicines: Implications for Policy and Practice
The current healthcare dynamic has shifted from one-size-fits-all to patient-centred care, with our increased understanding of pharmacokinetics and pharmacogenomics demanding a switch to more individualised therapies. As the pharmaceutical industry remains yet to succumb to the push of a technological paradigm shift, pharmacists lack the means to provide completely personalised medicine (PM) to their patients in a safe, affordable, and widely accessible manner. As additive manufacturing technology has already established its strength in producing pharmaceutical formulations, it is necessary to next consider methods by which this technology can create PM accessible from pharmacies. In this article, we reviewed the limitations of current pharmaceutical manufacturing methods for PMs, three-dimensional (3D) printing techniques that are most beneficial for PMs, implications of bringing this technology into pharmacy practice, and implications for policy surrounding 3D printing techniques in the manufacturing of PMs.
Introduction
It is well established that variation exists from one patient to another – enhanced knowledge in pharmacogenomics, individual pharmacokinetics, and a patient’s unique anatomy and physiology has formed the understanding that not one patient is or responds the same as another (Savard, 2013). Personalised medicine (PM), as opposed to currently available conventional medicines, is underpinned by the notion of patient-centred care, as the medication is produced with drug(s), dose(s), release kinetics, and formulation completely customised to suit the individual patient’s needs, as determined by the patient’s personal preferences and the prescribers understanding of the patient’s unique disease profile. Patient populations that most require personalisation include geriatrics , paediatrics (Bartelink et al., 2006), and overweight/obese patients (Cheymol, 2000), as often non-conventional doses are needed to account for their altered pharmacokinetic profiles, and modified dosage forms are required in cases of anatomical dysfunction, e.g. dysphagia (Aziz et al., 2022). Adverse drug reactions occur, especially in these populations, when their altered kinetics and needs are unaccounted for, with untailored therapy representing 75-85% of total adverse drug reaction cases (Alhnan et al., 2016). Currently, non-conventional doses are obtained via traditional, pharmacist-performed compounding. Many have raised the issue of poor on-site regulation and quality control, leading to increased dosing errors and cases of contamination (Drazen et al., 2012, Watson et al., 2021).
As the pharmaceutical industry remains yet to succumb to the push of a technological paradigm shift, health care professionals are left without the means to provide utterly personalised health care to their patients in a safe, affordable, and widely accessible manner. However, the three-dimensional (3D) printing of PMs offers pharmacy practice a novel solution to our current gap in patient-centred care; however, it does not come without implications. While previous reviews have explored the technical applications of 3D printing for pharmaceuticals (Afsana and V., Haider, N., Jain, K., , 2018, Anwar-Fadzil et al., 2022, Chen et al., 2020, Dumpa et al., 2021, Lim et al., 2018), none have investigated the impact on policy and practice. Thus, this review aims to discuss the feasibility of introducing 3D printing methods into pharmacy practice for PMs to become readily available to patients in the community. The study will specifically address technical methods in production, transitioning from experimentation to the consumer, and the resulting implications for practice and policy.
An initial screening of PubMed, Embase, Google Scholar, and Scopus was performed. Specific keywords included in the search were: three-dimensional printing (3d printing, 3-dimensional printing, additive manufacturing, digital manufacturing, layered manufacturing); PMs (individualised medicines, individualised therapy, personalised therapy, precision medicine); and Pharmacy Practice (clinical practice, pharmacy setting, pharmacy, chemist, compounding). The search included all types of studies and grey literature published from 2018 to 2022. Literature regarding bioprinting (e.g., 3D printing of tissues, prosthetics, and other medical implants) was excluded. Additionally, citation chaining was performed to ensure articles missed by the database searches were included.
Download the full article as PDF here 3D Printing for Personalised Medicines_Implications for Policy and Practice
or read it here
Klaudia Englezos, Lingxin Wang, Edwin Tan, Lifeng Kang, 3D Printing for Personalised Medicines: Implications for Policy and Practice, International Journal of Pharmaceutics, 2023, 122785, ISSN 0378-5173, https://doi.org/10.1016/j.ijpharm.2023.122785.

