Inhalable dry powder product (DPP) of mRNA lipid nanoparticles (LNPs) for pulmonary delivery
Abstract
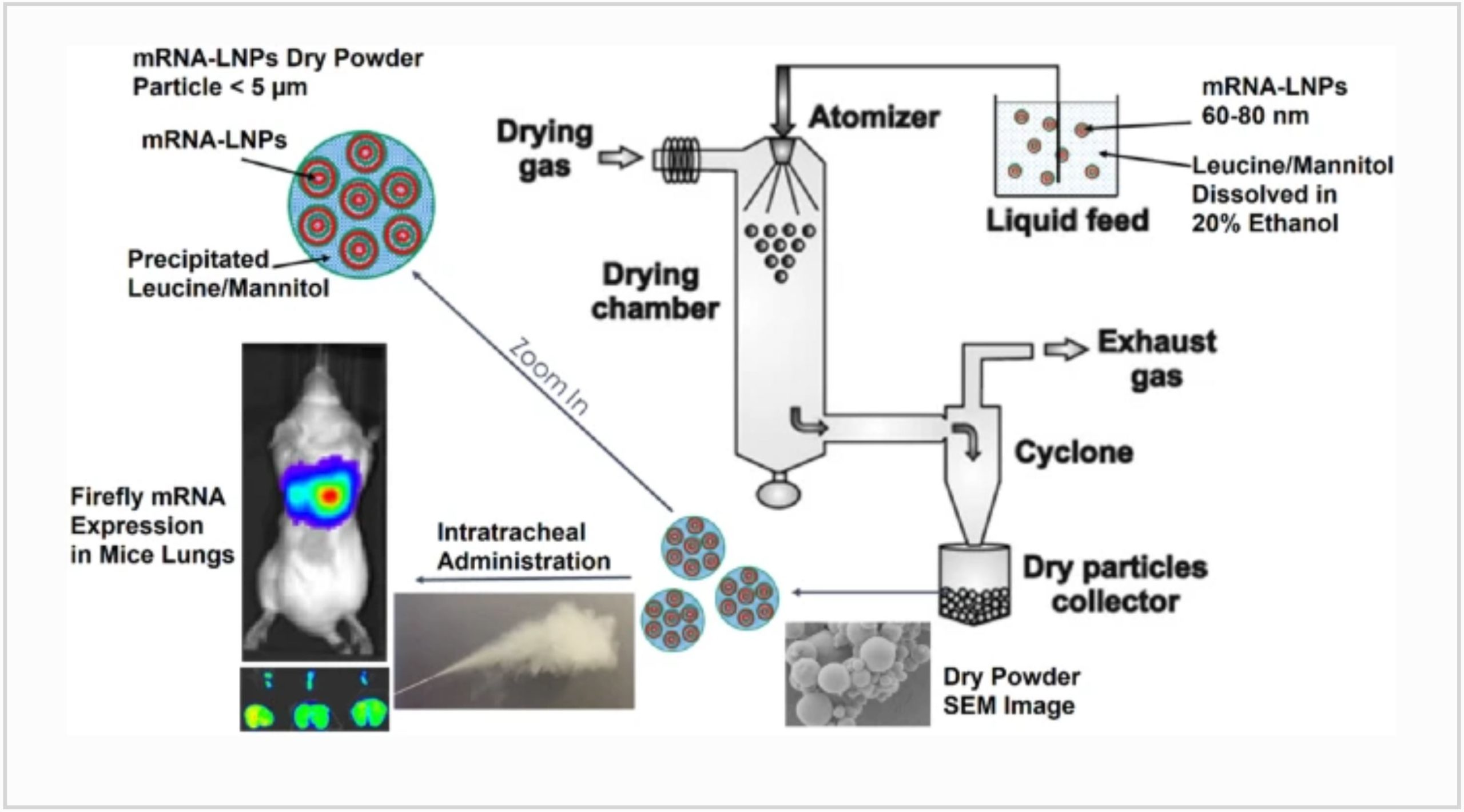
Pulmonary delivery of mRNA via inhalation is a very attractive approach for RNA-based therapy for treatment of lung diseases. In this work, we have demonstrated successful development of an mRNA-lipid nanoparticle (LNP) dry powder product (DPP), wherein the LNPs were spray dried using hydroalcoholic solvent along with mannitol and leucine as excipients. The desired critical attributes for the DPP were accomplished by varying the excipients, lipid composition, concentration of LNPs, and weight percentage of mRNA. Leucine alone or in combination with mannitol improved the formulation by increasing the mRNA yield as well as decreasing the particle size. Intratracheal administration of the DPP in mice resulted in luciferase expression in the trachea and lungs indicating successful delivery of functional mRNA. Our results show formulation optimization of mRNA LNPs administered in the form of DPP results in an efficacious functional delivery with great promise for future development of mRNA therapeutics for lung diseases.
Introduction
The rapid approval and remarkable success of Comirnaty (BNT162b2) and Spikevax (mRNA-1273) have demonstrated the clinical validation of mRNA as a new class of highly efficacious nucleic acids in the field of vaccines [1]. The mechanism by which an mRNA vaccine acts involves delivery of synthetically transcribed mRNA molecules that encodes for a viral protein to the human host cells [2]. The host cells then produce the viral protein that leads to adaptive immune response to fight the corresponding viral infection [3]. The application of mRNA extends beyond vaccines in the areas of protein replacement therapy for genetic diseases, gene editing, and oncology applications, as well as others [4]. Therapeutic treatments for liver and lung diseases are being developed by delivering synthetic mRNA to encode for and replace a missing or non-functional protein to the corresponding target cells via intravenous and inhalable routes, respectively [5,6,7]. Delivering mRNA to either the liver or lung for therapeutic application has its own benefits and challenges [8]. Since the focus of this work is on developing dry powder (DP) formulations for inhalation, mRNA therapeutics has been discussed in the context of pulmonary delivery.
A pulmonary route of administration for mRNA may be preferred due to numerous advantages. Delivering inhalable medication to the lungs is a non-invasive method and offers direct access to upper and lower airway epithelial cells as well as the alveoli and lung parenchyma along with hundreds of square meters of surface area rich in vasculature for fast distribution [9]. Successful delivery of mRNA to the target cells in the lungs may result in the successful treatment of pulmonary diseases such as acute respiratory distress syndrome (ARDS), cystic fibrosis (CF), lung cancer, pulmonary alveolar proteinosis (PAP), pulmonary arterial hypertension (PAH), and primary ciliary dyskinesia (PCD) [10].
Despite of its inherent advantages, successful lung delivery requires lot of work around optimization of both the formulation and inhalation devices [11]. Nebulizers, pressurized metered dose inhalers (pMDIs), and dry powder inhalers (DPIs) are three main types of inhalation devices that are used for drug administration to the lungs [12]. Although nebulizers can generate fine mist that exhibits efficient deposition deep into the lung tissue, such devices are less patient friendly primarily due to the longer duration of inhalation and difficulty in operating [13]. In addition, achieving and maintaining a high rate of nebulization as well as maintaining critical quality attributes and stability of the mRNA-LNP product throughout the inhalation period can be challenging [14]. On the other hand, pMDIs are easy to handle and are more reliable due to their consistent metering leading to accurate dosing [15]. However, they also come with compliance issues due to a requirement of hand-lung coordination by the patient [16]. In addition, there are efforts to reduce the carbon footprint of pMDIs as they require greenhouse gases like hydrofluoroalkanes as propellants to release the required dose at higher speed [17]. DPIs are the most advanced inhalation devices for lung delivery and can overcome some of the challenges associated with nebulizers and pMDIs [18]. They are less expensive, portable, do not require any propellants for delivery, can deliver higher doses in shorter period, can be actuated by breathing, and are easy to operate [19, 20]. There are several DPI devices available in the market such as Rotahaler, Diskus, Spiros, Turbuhaler, and Clickhaler that discharge DPP to breathe in easily by the patient [21]. Furthermore, DPP affords higher stability due to its solid state, which can be advantageous for mRNA delivery [22, 23].
The performance of DPP mostly depends on the number of particles deposited in the target areas of the lungs; undeposited particles are either exhaled out or swallowed showing no efficacy or unwanted side effects. Although there are several factors that can influence movement of DPP particles into the airways, aerodynamic particle size primarily determines the site and extent of deposition [24]. Ideally, the mass median aerodynamic diameter (MMAD) of DPP particles should be below 5 µm as particles in the range of 1 to 3 µm exhibit the highest deposition in the central and peripheral airways leading to sedimentation and subsequent absorption, whereas particles below 1 µm and above 5 µm are exhaled out or swallowed, respectively [25]. Other characteristics that can also play some role in DPP flow in the airways include bulk and tap density, moisture content, rate of water absorption, flowability, and surface area of the particles [26].
Spray drying, which involves atomization of solution into droplets followed by rapid evaporation, is a commonly used, economical and an established technique to manufacture the DPP for various modalities such as small molecules, peptides, and proteins. The operation is continuous, scalable, suitable for heat-sensitive material and can produce robust, consistent DPP with desired formulation characteristics [27]. Various sugars such as lactose and mannitol are commonly used as carrier excipients to facilitate the spray drying process [28]. Mannitol is an attractive excipient for spray drying of mRNA formulations showing beneficial properties which include (i) altering the effect on the viscoelastic properties associated to phlegm, (ii) increasing water content driven by osmotic gradient, (iii) less hygroscopic compared to some other sugars like lactose, and (iv) stability as a non-reducing sugar with absence of any aldehyde group. Recently, amino acids such as leucine, valine, isoleucine, and trileucine have been utilized to improve aerosolization properties of inhalable microparticles by increasing the dispersibility, decreasing agglomeration, and decreasing the MMAD of DPP [26, 29]. Inhalable formulations of mRNA with peptides or exosomes have been demonstrated previously [8, 30]. To the best of our knowledge, reports of excipient screening and optimization of formulation properties and aerosol performance of spray dried mRNA LNPs are rare. In continuation of our efforts of developing dry powder formulation for mRNA delivery [31], herein, we report successful formulation optimization work of spray drying two types of LNP formulations in hydroalcoholic solutions made using novel ionizable lipids in combinations with mannitol and leucine as excipients. We have designed novel ionizable lipid families based of phenolic acid and citric acid cores that have shown promise in pulmonary delivery of mRNA [32, 33]. In this work, we have evaluated two such novel ionizable lipids: lipid A based on phenolic acid core and lipid B based on citric acid core (Fig. S1). Both lipids have ester linkers, making them potentially biodegradable and thus a lower risk of safety concerns. We demonstrate functional dry powder formulation of mRNA-LNPs with desired characteristics can be successfully formulated using spray drying technique by optimizing the solvents, excipient combinations, processing parameters, and LNP composition.
Download the full article as PDF here Inhalable dry powder product (DPP) of mRNA lipid nanoparticles (LNPs) for pulmonary delivery
or read it here
Sarode, A., Patel, P., Vargas-Montoya, N. et al. Inhalable dry powder product (DPP) of mRNA lipid nanoparticles (LNPs) for pulmonary delivery. Drug Deliv. and Transl. Res. (2023). https://doi.org/10.1007/s13346-023-01402-y
Read more articles about “Dry Powder Inhalers (DPI)” here:
- Development of inhalation powders containing lactic acid bacteria with antimicrobial activity against Pseudomonas aeruginosa
- Complexities related to the amorphous content of lactose carriers
- Supercritical antisolvent-fluidized bed for the preparation of dry powder inhaler for pulmonary delivery of nanomedicine