Orally disintegrating drug carriers for paediatric pharmacotherapy
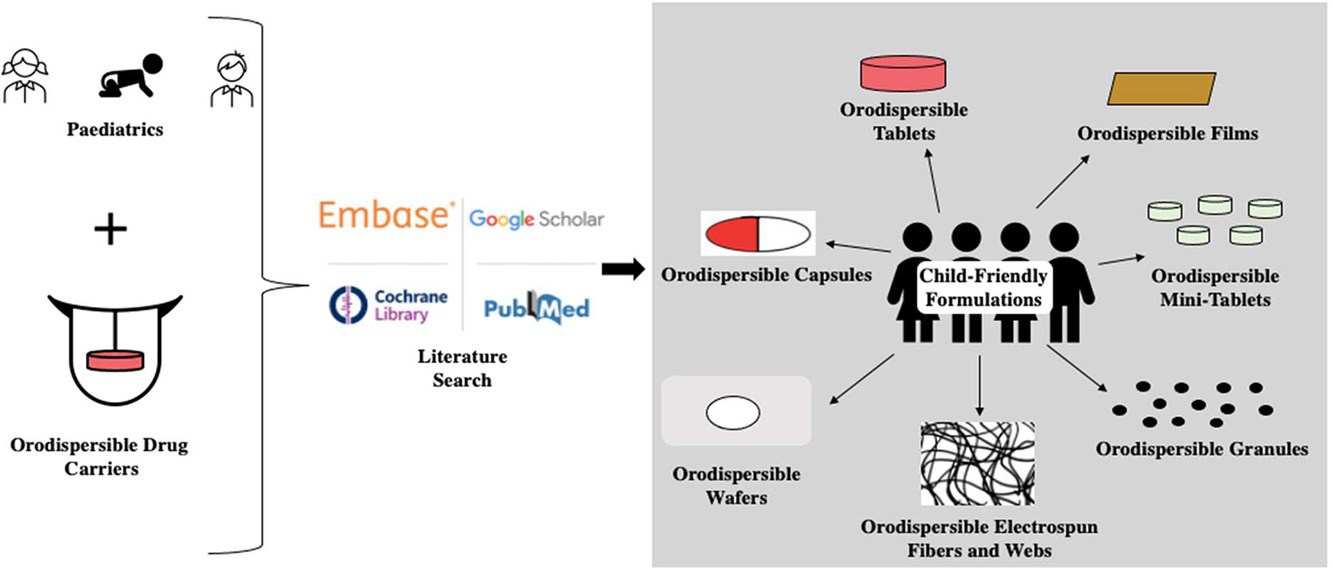
Non-compliance, dosing inaccuracy, choking risk, flavour, and instability, are some of the issues associated with paediatric, oral dosage forms — tablets, capsules, solutions, and suspensions. Orally disintegrating drug carriers, a dosage form with growing interest, are thought to overcome several of the challenges associated with these conventional formulations by rapidly disintegrating within the buccal cavity without the need for water. This review serves as an up-to-date report on the various types of orodispersible delivery systems, currently being developed or commercialized, by detailing their characteristics, manufacturing processes, and applications in the paediatric population.
Mentioned are orodispersible tablets, films, wafers and lyophilisates, mini-tablets, capsules, granules, electrospun fibers and webs. Also highlighted are the choice of excipients, quality control requirements, and expected pharmacokinetics of orally disintegrating drug carriers concerning the paediatric population. Overall, orodispersible formulations, particularly tablets, films, and lyophilisates/wafers, have shown to be a valuable addition to medication administration in minors, thus the execution of more targeted research and development activities is expected to lead to enhanced paediatric care and outcomes.
2.2. Orodispersible films
2.2.1. Overview
Orodispersible films (ODFs) are single or multilayered sheets containing appropriate ingredients that rapidly disperse when placed in the mouth (Gupta et al., 2021). They are most commonly rectangles or squares; however, circles and U-Shaped ones exist (Gupta et al., 2021). They inherently have a larger surface area than ODTs and as such, often have faster disintegration time (Özakar and Özakar, 2021). They are also often easier to handle, and store compared to ODTs since they are generally less brittle. ODFs are used for local action in the oral cavity for disease states like ulcers or cold sores. They are also used for systemic effects to treat several disease states (Mahboob et al., 2016). Recently, Klingmann et al. compared the acceptability of ODFs compared to syrups in neonates and infants (Klingmann et al., 2020). The authors showed that ODFs are both a safe and effective dosage form for this population.
2.2.2. Manufacture process
Like ODTs, several methods currently exist for producing orally disintegrating films. These include:
2.2.2.1. Casting method
This method is commonly used due to its low cost and simplicity. The solvent casting method relies on the use of heated magnetic stirrer to prepare a viscous solution containing water soluble drug(s) and excipients. The viscous solution is first of all cast using specialized molds or petri dishes with specific dimensions and then left at room temperature over a period of time (usually 24 – 48 h) or sometimes in an oven set at 40 – 50°C to allow evaporation of the solvents (Mahboob et al., 2016; Özakar and Özakar, 2021). The resulting films (with specific dimensions — diameter and thickness) can then be cut to the desired dimensions (Slavkova and Breitkreutz, 2015). Similarly, the semisolid casting method involves the creation of a viscous solution (from the drug and gel forming polymeric excipients) which is poured into specific molds, allowed to solidify into a pliable mass which can then be cut to the desired size (Mahboob et al., 2016). Generally, batch-to-batch variations in film thickness is inevitable while using this method, it requires a significantly long drying period and is not suitable for preparing films larger than 25 – 30 cm, making scale-up/large scale production problematic (Palezi et al., 2022).
2.2.2.2. Extrusion
Extrusion can generally be described as either hot-melt extrusion or solid-dispersion extrusion (Mahboob et al., 2016). Using hot-melt extrusion, the drug and excipients are mixed in the dry state and heated until fluid using an extruder. (Mahboob et al., 2016; Reza and Chakraborty, 2016; Özakar and Özakar, 2021). The molten mixture is then expelled through the sheet-die hole while being pulled at a constant speed and wound up on a roll. Once cooled, the roll of film can then be cut to desire a length/dimensions (Richter, 2019). Solid-dispersion extrusion, on the other hand, involves the incorporation of a drug containing wet powder blend with a heated hydroalcoholic solvent. Thereafter, the resultant solid dispersion is then molded into the desired film structure. The extrusion technique allows uniform distribution of the active drugs and reduced operation units thus decreasing the production steps and allowing continuity which makes it a more desirable process for large scale ODF production. However, the extrusion technique is only suitable for non-thermolabile drugs since the drug mixture needs to be heated at high temperatures (Mahboob et al., 2016; Özakar and Özakar, 2021). Also, it has limited value in the production of ODFs given that most polysaccharides, an important excipient in ODFs, are heat sensitive and/or can exhibit an elevated glass transition temperatures that is not usually easy to adjust with the inclusion of plasticizers, thus resulting in the formation of very sticky or ductile films (Musazzi et al., 2020; Palezi et al., 2022)
2.2.2.3. Rolling method
For this method, the drug, film forming polymers, other excipients, and solvents are combined to form a solution or suspension often referred to as the “premix” or “master batch”. A predetermined amount of this master batch is then transferred onto a roller drum, rolled, and left to dry using the controlled bottom drying approach, without external air currents or heat on the film surface. Post drying, the ODF is formed which are then cut to the desired sizes, shapes, and thicknesses. The film thickness is controlled with a metering roller and the solvent used is usually water or a mixture of water and alcohol. Obtaining uniform film thickness and proper sample drying can be quite challenging for this method (Mishra and Amin, 2011; Mandeep et al., 2013; Reza and Chakraborty, 2016; Salawi, 2022).
2.2.2.4. Printing technologies
A more recent approach to formulating ODFs involves the use of two-dimensional (2D) or three-dimensional (3D) printing technology for formulating drug containing ODFs (Öblom et al., 2019). Briefly, the process involves first preparing a polymer/excipient blend without the active drug which is generally used later as the substrate for printing the drug containing solution or suspension with a printer. Films are usually printed one at a time, and left to dry overnight (Öblom et al., 2019; Palezi et al., 2022). Since this approach involves the delayed deposition of the active drug on the excipient substrate using the printer, this helps preserve the drug from thermal or mechanical degradative stress associated with the production and drying phases. This technique can be used for preparing polymeric matrices that are useful for the encapsulation of precise amounts of drugs/bioactive agents and, production can be done on demand, thus offering a unique way of making ODFs for individualized therapy. Printing technologies are limited by the high costs and time required, often leading to only small quantities being prepared per time (Musazzi et al., 2020; Palezi et al., 2022).
2.2.3. Application in paediatric drug formulation
There are currently several research groups working on developing ODFs with the paediatric population in mind. Senta-Loys et al. sought to design tetrabenazine ODFs for the treatment of hyperkinetic movement disorders in paediatrics (Senta-Loys et al., 2017). Before this effort, no paediatric-approved drug form of tetrabenazine existed so crushed tablets were used. They prepared the tetrabenazine ODFs using the casting/evaporation method. To do so, a gel, containing a film-forming polymer, excipients, and tetrabenazine, was cast onto a petri dish and dried. The final step involved cutting the films such the final product had a surface area of 4 cm2.
Additionally, Preis et al. designed ODFs of dimenhydrinate, for use in paediatrics, as an alternative to its marketed formulations — tablets, syrups, and suppositories. The researchers determined the disintegration time of the dimenhydrinate ODFs to be between below one minute and below 2 min for the petri dish and drop method, respectively (Preis and Breitkreutz, 2012).
Due to the shortage of paediatric-specific tuberculosis drug formulations, Matawo et al. designed pyrazinamide containing ODFs for the treatment of tuberculosis in children (Matawo et al., 2020). Using the solvent casting method, the pyrazinamide ODF was prepared with varying amounts of excipients. The optimized ODF was found to disintegrate in less than 60 s in addition to being flexible, thin, and easy to handle. The authors concluded that the developed formulation offered a potential solution to the several current challenges preventing the successful treatment of tuberculosis in the paediatric population.
Despite warfarin, a narrow therapeutic index drug, being used in several instances to prevent thrombotic events in paediatrics, there are currently no available paediatric-specific drug formulations (Öblom et al., 2019). Öblom and co-workers aimed to investigate the issue by comparing the traditional dosage form, oral powders in unit dose sachets (OPSs), to ODFs. In terms of dose uniformity, the prepared ODFs were found to be superior to the conventional OPSs. Interestingly, the authors were able to print QR codes on the ODFs using edible ink; the QR codes could be used to avoid medication errors. The authors reported the use of warfarin containing ODFs prepared by printing methods would be advantageous, especially in hospital settings, by offering personalized medicine to the paediatric population.
Knowing that often drug formulations require more than one API, Thabet et al. (2018b) aimed to produce a multi-layered ODF containing both enalapril and hydrochlorothiazide. The researchers used the solvent casting method to prepare the multi-layer ODF; it was found that using different polymers between the film layers decreased the migration of the APIs between the layers. The production of multi-drug-containing formulations offers several possible advantages in the paediatric population, including increased compliance and therapy effectiveness.
ODFs can be prepared using hot-melt extrusion, but this technique is limited by the hot temperatures required which often results in the exclusion of thermosensitive drugs (Khalid et al., 2021). To investigate hot-melt extrusion, Khalid et al. (2021) used diclofenac sodium, a thermosensitive drug, to prepare ODFs intended for the paediatric population. The preparation involved leaving the diclofenac-containing paste in a heated chamber at 95°C for 10 min so the melted mixture could be printed and packaged. The authors concluded the hot-melt extrusion was a useful method to prepare diclofenac ODFs and could likely be applied to other thermosensitive drugs.
2.6. Orodispersible mini-tablets
2.6.1. Overview
Orodispersible mini-tablets (ODMTs) are solid dosage forms generally with a diameter of 2 – 4 mm, a surface-to-volume ratio of at least 2 mm−1, and an aspect ratio of approximately one (Comoglu and Ozyilmaz, 2019; Lura et al., 2021). In addition to these characteristics, ODMTs also have the distinguishing feature of all orodispersible drug carriers whereby they disintegrate in the oral cavity in 30 – 180 s. Compared to ODTs, the small size of ODMTs increases the acceptability of the dosage form in the paediatric patients. ODMTs with diameters between 2 – 3 mm diameters have been shown to be suitable for children who are six months to eight years of age, respectively. ODMTs are useful for infants and toddlers requiring weight-based dosing due to the high dosing flexibility of the dosage form. One limitation of ODMTs is the very limited drug loading capacity, often resulting in the patient being required to take multiple ODMTs (El-Say et al., 2015; Comoglu and Ozyilmaz, 2019; Lura et al., 2019; Wiedey et al., 2021).
2.6.2. Manufacture process
The manufacturing process of ODMTs is largely the same as ODTs, including direct compression and granulation (Soulairol et al., 2018; Kokott et al., 2021). Stoltenberg et al. was of one of the first groups to construct ODMTs with the paediatric population in mind (Stoltenberg and Breitkreutz, 2011). To prepare the ODMTs, hydrochlorothiazide and five commercially available excipients, that contained mannitol as the main component, were used. Using direct compression, the various powder mixtures were compressed into biconvex mini-tablets with a diameter of 2 mm.
2.6.3. Application in paediatric drug formulation
Currently, there are no commercially available ODMTs on the market, but several projects are in the works (Slavkova and Breitkreutz, 2015; Khan et al., 2021). El-Say et al. worked to develop risperidone ODMTs for paediatric use (El-Say et al., 2015). They used direct compression to prepare risperidone 5 mg ODMTs with a 2 mm diameter. Using statistical optimization, the researchers deemed the ODMTs to be a successful formulation based on having sufficient mechanical strength, uniformity of mass, a rapid disintegration time, and minimal friability. Another instance of ODMTs being developed for paediatric use is with enalapril maleate for the treatment of hypertension (Ortega et al., 2020). Hypertension is a serious condition in paediatrics, consequently, children-specific drug formulations are necessary. Ortega and team successfully designed an optimal ODMT formulation containing enalapril maleate drug as a model using varying lactose co-pressed excipients by direct compression (Ortega et al., 2020). The enalapril maleate loaded ODMT was completely disintegrated within 28 s and considered suitable for further development and manufacturing.
Download the full article as PDF here Orally disintegrating drug carriers for paediatric pharmacotherapy
or read it here
Emma A. Kean, Oluwatoyin A. Adeleke, Orally disintegrating drug carriers for paediatric pharmacotherapy, European Journal of Pharmaceutical Sciences, Volume 182, 2023, 106377, ISSN 0928-0987, https://doi.org/10.1016/j.ejps.2023.106377.
Our next webinar:
For free registration and more information click on the picture below or here: